Stopping heavy bleeding with next-generation artificial platelets

Case Western Reserve University researchers develop next generation of artificial platelets that can stop bleeding from an injury faster
Biomedical researchers at Case Western Reserve University report that their latest innovation in developing synthetic platelets could help save lives by rapidly stabilizing clots to reduce blood loss from traumatic injuries.
This new effort centers on the creation of next-generation, platelet-mimicking nanoparticles. These particles help generate a protein mesh that acts as a natural netting to stabilize blood clots and help stop bleeding.
If proven safe and efficient in clinical trials, the technology would bolster the scientists’ advances in a decade-long effort to develop and optimize what they call synthetic platelet surrogates.

Anirban Sen Gupta
“This is the next step in artificial-platelet technology and it’s truly a critical advance,” said Anirban Sen Gupta, a professor of biomedical engineering at Case Western Reserve, who led the new research. “We have not only been able to form a plug to reduce bleeding from a traumatic injury, but to also help form fibrin, a protein mesh that secures the plug, further stabilizing the clot.”
Sen Gupta and his team have for the last decade pioneered research in artificial platelet systems. They have worked on therapeutic technologies with applications in hemostasis (stopping bleeding), thrombolysis (breaking harmful blood clots) and inflammation (numerous blood cell-related pathologies).
The researchers detailed their findings in a paper published this month in the journal Science Translational Medicine.
They reported that the nanoparticles helped the clot form faster and stop bleeding in animal models, even when natural platelets were significantly depleted. They refer to the particles as “platelet-mimicking procoagulant nanoparticles” (PPNs).
Platelets and bleeding
Blood has four main components: plasma, red blood cells, white blood cells and platelets. Platelets help the blood-clotting process by quickly gathering at the site of an injury. They also stick to the lining of the injured blood vessel, clustering to form a plug. Finally, they amplify the formation of fibrin, an insoluble protein mesh that slows bleeding.
Medical professionals use platelet transfusions to prevent or treat bleeding complications in trauma, surgery and various clotting disorders. They use more than 2 million platelet units each year in the United States, according to the Red Cross.
However, natural platelets aren’t always available or portable and have a limited shelf life. This has prompted research over the last several decades into synthetic alternatives.
The new technology
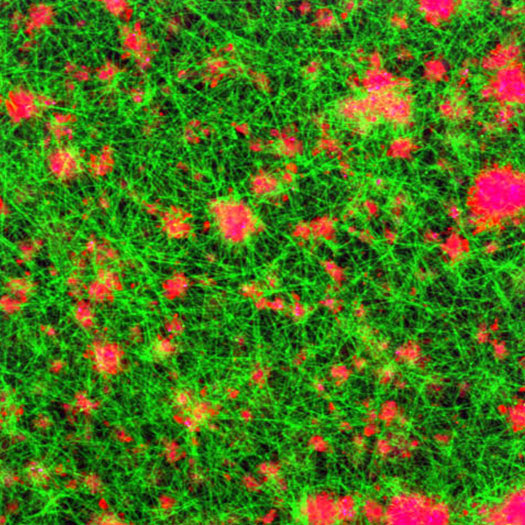
A scanning electron microscopy image of a blood clot. The green mesh is the fibrin and the pink areas are the PPNs.
These promising results suggest that this new nanoparticle design could further enhance the performance of artificial platelet technologies that Sen Gupta and his research team have been working to develop over the last decade.
That team’s first-generation design has proven to mimic two functions of natural platelets, Sen Gupta said.
The first is a type of “homing” mechanism that helps platelets sense and then stick to a bleeding injury. The second is the ability of platelets to pile up on each other to form a plug, like stacking sandbags as a barrier that stops a flood—in this case bleeding.
“But to ensure that the sandbags stay put under the force of flood, you would need netting to secure them,” Sen Gupta said. “Then, you would need to peg the netting down so it wouldn’t move. Fibrin is this netting, and we have shown that the PPNs can amplify formation of fibrin even when natural platelets are depleted.”
Sen Gupta said that this suggests that PPNs can be used as a viable platelet surrogate. Medical professionals could use the material to stop bleeding when natural platelet transfusion products are limited.
Sen Gupta and Ujjal Didar Singh Sekhon, a former PhD student in his lab, were the primary authors on the paper. Several collaborators joined in the work, including Marvin Nieman, associate professor of pharmacology at the Case Western Reserve School of Medicine. Matthew Neal, director of the Pittsburgh Trauma and Transfusion Medicine Research Center at the University of Pittsburgh, also was a key contributor.
Sekhon graduated in 2021 and now works at by Haima Therapeutics, a biotechnology company that Sen Gupta co-founded in 2016 to commercialize technologies developed at Case Western Reserve.
The National Institutes of Health (NIH) supported the research with a $2.1 million, four-year grant awarded in 2021 to Sen Gupta (along with collaborators at the University of Michigan and University of North Carolina) to advance the design of artificial platelets.
For more information, contact Mike Scott at mike.scott@case.edu.

